Comorbid psychiatric disorders refer to the occurrence of two or more psychiatric conditions simultaneously in an individual. This phenomenon is common and poses significant challenges in diagnosis, treatment, and overall management of mental health. Comorbidity can complicate the clinical picture, often leading to poorer outcomes, increased healthcare utilization, and greater overall impairment. Understanding the intricacies of comorbid psychiatric disorders is essential for healthcare providers, patients, and their families to navigate the complexities of mental health care.
Definition and Prevalence
What is Comorbidity?
Comorbidity in psychiatry refers to the co-occurrence of two or more mental disorders in the same individual. This can involve a combination of conditions such as depression and anxiety, schizophrenia and substance use disorder, or bipolar disorder and post-traumatic stress disorder (PTSD). The interaction between these disorders can exacerbate symptoms, complicate treatment, and impact the individual’s quality of life significantly.
Statistical Prevalence
Research indicates that comorbidity is more the rule than the exception in psychiatric populations. Studies have shown that nearly half of those diagnosed with one mental disorder will meet the criteria for another at some point in their lives. For instance, the National Comorbidity Survey Replication (NCS-R) found that approximately 45% of individuals with one psychiatric disorder met criteria for two or more additional disorders. This high prevalence underscores the importance of recognizing and addressing comorbid conditions in clinical practice.
Common Comorbid Psychiatric Disorders
Depression and Anxiety
Depression and anxiety disorders frequently co-occur. Individuals with major depressive disorder (MDD) often experience anxiety disorders such as generalized anxiety disorder (GAD), panic disorder, or social anxiety disorder. The presence of both conditions can intensify the symptoms of each, leading to more severe depression, greater functional impairment, and a higher risk of suicide.
Bipolar Disorder and Substance Use Disorder
Bipolar disorder is commonly associated with substance use disorders (SUD). The impulsivity and risk-taking behaviors during manic or hypomanic episodes can lead to substance abuse as individuals seek to self-medicate or enhance their mood. Conversely, substance use can trigger or worsen manic and depressive episodes, creating a vicious cycle that complicates treatment and prognosis.
Schizophrenia and Depression
Depression is prevalent among individuals with schizophrenia, contributing to poorer outcomes, including higher rates of relapse, hospitalization, and suicide. Negative symptoms of schizophrenia, such as anhedonia and social withdrawal, can overlap with depressive symptoms, making diagnosis and treatment challenging.
PTSD and Borderline Personality Disorder
Post-traumatic stress disorder (PTSD) and borderline personality disorder (BPD) often co-occur, particularly in individuals with a history of trauma. The emotional dysregulation, intense interpersonal conflicts, and identity disturbances seen in BPD can be exacerbated by the re-experiencing, hyperarousal, and avoidance symptoms of PTSD, leading to significant distress and impairment.
Causes and Risk Factors
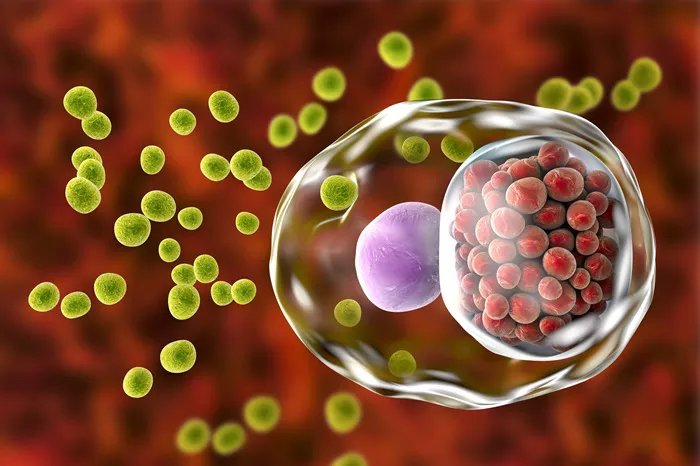
Genetic and Biological Factors
Genetic predispositions play a crucial role in the development of comorbid psychiatric disorders. Shared genetic factors may contribute to the susceptibility of multiple disorders. For example, genetic variations affecting neurotransmitter systems such as serotonin, dopamine, and norepinephrine can influence the risk of both depression and anxiety disorders.
Environmental Influences
Environmental factors, including childhood adversity, trauma, and chronic stress, are significant contributors to the development of comorbid psychiatric conditions. Early life stressors can disrupt neurodevelopment and increase vulnerability to multiple mental health issues later in life. Additionally, socio-economic factors, such as poverty and lack of access to healthcare, can exacerbate these risks.
Psychological and Behavioral Factors
Psychological and behavioral patterns, such as maladaptive coping mechanisms and personality traits, can also contribute to comorbidity. For instance, individuals with high neuroticism are more likely to experience anxiety and depression simultaneously. Similarly, those with impulsive or risk-taking behaviors may be predisposed to both substance use disorders and mood disorders.
Diagnostic Challenges
Overlapping Symptoms
The overlap of symptoms between different psychiatric disorders presents a significant challenge in diagnosis. For instance, symptoms like fatigue, concentration difficulties, and sleep disturbances are common in both depression and anxiety disorders. This overlap can lead to misdiagnosis or underdiagnosis, delaying appropriate treatment.
Diagnostic Criteria and Tools
The current diagnostic criteria, as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), aim to provide clear guidelines for identifying individual disorders. However, the presence of comorbid conditions often complicates the diagnostic process. Clinicians must use comprehensive assessment tools, including structured interviews and validated questionnaires, to accurately identify all co-occurring disorders.
Importance of Comprehensive Assessment
A thorough and comprehensive assessment is essential for accurately diagnosing comorbid psychiatric disorders. This involves taking a detailed history of the patient’s symptoms, past psychiatric diagnoses, family history, and psychosocial factors. A multi-disciplinary approach, involving psychiatrists, psychologists, and other mental health professionals, is often necessary to obtain a complete understanding of the patient’s condition.
Treatment Approaches
Integrated Treatment Models
Integrated treatment models that address both or all co-occurring disorders simultaneously are considered the gold standard in managing comorbid psychiatric conditions. These models emphasize coordinated care, where mental health professionals work collaboratively to develop and implement a treatment plan that addresses all aspects of the patient’s mental health.
Pharmacotherapy
Pharmacological treatment must be carefully tailored to manage multiple disorders. This often involves using medications that target common pathways implicated in the co-occurring conditions. For instance, selective serotonin reuptake inhibitors (SSRIs) are effective in treating both depression and anxiety. However, polypharmacy, or the use of multiple medications, may be necessary in some cases, requiring careful monitoring for potential drug interactions and side effects.
Psychotherapy
Psychotherapeutic interventions, such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and trauma-focused therapies, are essential components of treatment. These therapies can be adapted to address the unique needs of individuals with comorbid conditions. For example, DBT, which was originally developed for BPD, has been found effective in treating individuals with BPD and PTSD.
Lifestyle and Self-Management Strategies
Lifestyle modifications and self-management strategies play a crucial role in managing comorbid psychiatric disorders. Regular physical activity, healthy eating, adequate sleep, and stress management techniques can improve overall well-being and reduce symptom severity. Additionally, self-help groups and peer support can provide valuable resources and encouragement for individuals dealing with multiple mental health challenges.
Implications for Healthcare Providers
Training and Education
Healthcare providers must receive adequate training and education on the complexities of comorbid psychiatric disorders. This includes understanding the interplay between different conditions, recognizing the signs and symptoms of comorbidity, and being knowledgeable about the most effective treatment approaches.
Collaborative Care Models
Collaborative care models, which involve a team of healthcare providers working together to manage patient care, are essential in treating comorbid psychiatric disorders. These models facilitate communication and coordination between primary care physicians, psychiatrists, psychologists, social workers, and other healthcare professionals, ensuring that all aspects of the patient’s mental health are addressed.
Patient-Centered Care
Adopting a patient-centered approach is crucial in managing comorbid psychiatric disorders. This involves actively involving patients in their treatment planning, considering their preferences and values, and empowering them to take an active role in their care. Regular follow-ups and ongoing support are essential to monitor progress and make necessary adjustments to the treatment plan.
Challenges and Future Directions
Stigma and Access to Care
Stigma associated with mental health disorders remains a significant barrier to seeking and receiving appropriate care. This is particularly true for individuals with comorbid conditions, who may face additional stigma and discrimination. Efforts to reduce stigma and improve access to mental health services are crucial in addressing the needs of this population.
Research and Innovation
Ongoing research is essential to better understand the mechanisms underlying comorbid psychiatric disorders and to develop more effective treatments. Advances in neuroscience, genetics, and pharmacology hold promise for improving our understanding of these complex conditions and for developing targeted interventions.
Personalized Medicine
The future of psychiatric care lies in personalized medicine, which tailors treatment to the individual’s unique genetic, biological, and psychosocial profile. This approach has the potential to improve outcomes for individuals with comorbid psychiatric disorders by providing more precise and effective interventions.
Conclusion
Comorbid psychiatric disorders present significant challenges but also opportunities for advancing mental health care. By understanding the prevalence, causes, diagnostic complexities, and treatment approaches for these conditions, healthcare providers can offer more effective and comprehensive care. Through integrated treatment models, collaborative care, and ongoing research, we can improve the quality of life for individuals living with multiple psychiatric disorders and move towards a more holistic and patient-centered approach in mental health care.
[inline_related_posts title=”You Might Be Interested In” title_align=”left” style=”list” number=”6″ align=”none” ids=”9031,8959,8955″ by=”categories” orderby=”rand” order=”DESC” hide_thumb=”no” thumb_right=”no” views=”no” date=”yes” grid_columns=”2″ post_type=”” tax=””]