Latex allergies have become a significant health concern, particularly in healthcare environments and industries where latex products are frequently used. Understanding the types of latex that commonly cause allergies, the sources of exposure, and effective prevention strategies is crucial for minimizing risks and protecting those affected. This comprehensive article delves into the scientific and practical aspects of latex allergies, providing vital information for both healthcare professionals and the general public.
Latex and Latex Allergies
Latex is a natural product derived from the sap of the rubber tree, Hevea brasiliensis. It is widely used because of its exceptional elasticity, durability, and resistance. However, for some individuals, exposure to certain types of latex can trigger allergic reactions, which range from mild skin irritation to severe, life-threatening anaphylaxis.
Understanding Natural Rubber Latex
Natural rubber latex (NRL) is the primary type of latex that causes allergic reactions. This section explores its composition, use, and why it poses allergenic risks.
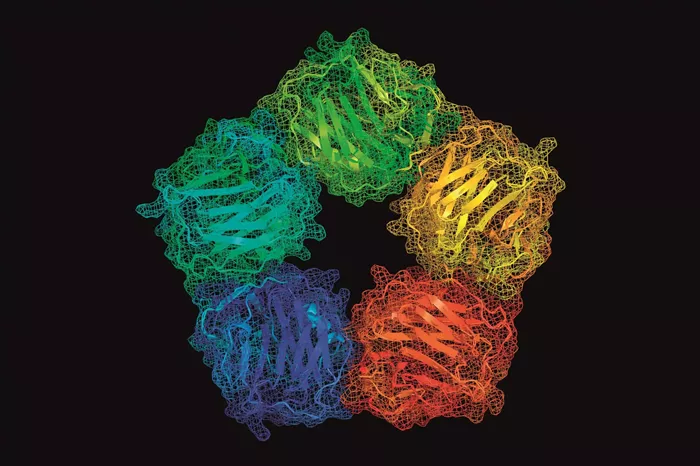
Composition and Allergenic Proteins: NRL is a milky fluid composed of lipids, phospholipids, proteins, and carbohydrates. The allergenicity of NRL is primarily attributed to its protein content, with over 60 different latex proteins identified, some of which can provoke severe allergic reactions.
Common Uses of NRL: NRL is used in various products, including medical gloves, balloons, rubber bands, and condoms. The widespread use of NRL in everyday items significantly increases the exposure risk, making it a public health concern.
Types of Latex Allergies
Latex allergies can be classified into three main types, each involving different immune mechanisms and presenting distinct symptoms. Understanding these types can help in diagnosing and treating the condition effectively.
Type I Allergy (Immediate Hypersensitivity): This is the most severe form of latex allergy and involves an immediate reaction mediated by IgE antibodies. Exposure to latex proteins can lead to symptoms ranging from hives and itching to anaphylaxis, a potentially life-threatening condition.
Type IV Allergy (Delayed Hypersensitivity): This type involves a delayed reaction mediated by T-cells, usually occurring 24-48 hours after exposure. Symptoms include redness, itching, and blistering at the contact site.
Irritant Dermatitis: Though not an allergic reaction, irritant dermatitis can be caused by latex products. It results from the direct irritation of the skin by chemicals in latex products rather than an immune response.
Risk Factors for Developing Latex Allergies
Certain individuals are at a higher risk of developing latex allergies. Identifying and understanding these risk factors can help in preventive measures and early diagnosis.
Healthcare Workers: Due to frequent and prolonged use of latex gloves and other medical supplies containing NRL, healthcare workers are particularly at high risk.
Patients with Spina Bifida: Individuals with spina bifida are often exposed to latex products through multiple surgeries and medical procedures, increasing their risk of sensitization.
Workers in the Rubber Industry: Those involved in the manufacturing of latex products are also at an increased risk due to high levels of airborne latex particles.
History of Multiple Surgeries: Frequent surgical interventions, especially in early childhood, can lead to increased exposure and higher sensitization rates to latex.
Diagnosis of Latex Allergies
Accurate diagnosis of latex allergies is essential for effective management. This section outlines the diagnostic methods used to confirm latex allergies.
Medical History and Physical Examination: Initial diagnostic steps involve a detailed medical history and physical examination, focusing on symptoms and exposure history.
Skin Prick Test (SPT): SPT is commonly used to detect Type I latex allergies. It involves applying a small amount of latex allergen to the skin and observing for an allergic reaction.
Specific IgE Blood Test: This test measures the level of latex-specific IgE antibodies in the blood, confirming a Type I allergy.
Patch Test: Used for diagnosing Type IV allergies, this test involves applying a patch containing latex to the skin for 24-48 hours to observe for a delayed reaction.
Prevention and Management of Latex Allergies
Preventing exposure to latex is crucial for individuals with latex allergies. This section provides strategies to minimize risk and manage reactions.
Use of Non-Latex Alternatives: Substituting latex products with non-latex alternatives, such as nitrile or vinyl gloves and silicone or polyurethane medical devices, can significantly reduce the risk of allergic reactions.
Latex-Free Policies: Implementing latex-free policies in high-risk settings, such as hospitals and clinics, can protect sensitive individuals.
Education and Awareness: Educating healthcare workers, patients, and the general public about the risks associated with latex exposure and the importance of allergy prevention strategies is essential.
Emergency Preparedness: Individuals with severe latex allergies should carry epinephrine auto-injectors and wear medical alert bracelets to ensure prompt treatment in the event of anaphylaxis.
Conclusion
Understanding the types of latex that commonly cause allergies, particularly natural rubber latex, is vital for developing effective strategies to prevent and manage these reactions. By recognizing the risk factors and implementing rigorous preventative measures, it is possible to protect those at risk and ensure safer environments for both healthcare workers and patients. Continued research and education are essential to further reduce the incidence of latex allergies and improve the quality of life for affected individuals.
[inline_related_posts title=”You Might Be Interested In” title_align=”left” style=”list” number=”6″ align=”none” ids=”8372,8369,8365″ by=”categories” orderby=”rand” order=”DESC” hide_thumb=”no” thumb_right=”no” views=”no” date=”yes” grid_columns=”2″ post_type=”” tax=””]