A major review into cervical screening at Southern Health Trust has revealed that eight women developed cancer after their smear tests were misread. The review, which assessed cases over a 13-year period, also found that 11 other women had pre-cancerous changes in their cells, requiring further treatment.
The findings have sparked outrage and concern, with campaigners calling for accountability and a public inquiry into the scandal. The Southern Health Trust has issued an apology to the affected women.
Review of Smear Test Failures
The review was prompted by the investigation into three women’s diagnoses, which were classified as Serious Adverse Incidents. Tragically, two of the women, Lynsey Courtney and Erin Harbinson, have since passed away. In total, over 17,000 women were asked to have their smear tests rechecked.
The investigation focused on two groups of women. The first group consisted of 207 women who had been diagnosed with cervical cancer. Eight women in this cohort developed cancer after their smear tests were misread. The review suggested that earlier diagnosis could have been made if the tests had been correctly interpreted.
The second group comprised 17,425 women whose tests were rechecked. Eleven of these women were found to have non-cancerous pre-cancerous changes in their cells and are currently undergoing treatment.
While the trust stated that it could not definitively link the misread tests to the development of cancer, the findings highlighted serious concerns regarding the accuracy of cervical screening at the trust.
Widespread Failures in Screening Process
The review revealed that underperformance by some screeners, combined with inadequate management oversight, led to these errors. Many of the affected women were failed by a system that failed to address the issues over an extended period.
Stella McLoughlin, a member of the advocacy group Ladies with Letters, described the situation as “unforgivable” and called for a public inquiry. She criticized the lack of accountability for the screeners involved and the ongoing failure to manage the process correctly.
“This has been an absolute scandal from start to finish,” McLoughlin said. “Smears being misread, people not being held to account, screeners not being managed properly – all of this is affecting real people.”
Action Taken by Southern Health Trust
In response to the review, the Southern Health Trust apologized to the affected families and acknowledged the distress caused. Dr. Steve Austin, the trust’s medical director, stated that the vast majority of smear tests reviewed were found to be normal. However, he recognized the emotional and physical toll on the women who received incorrect readings.
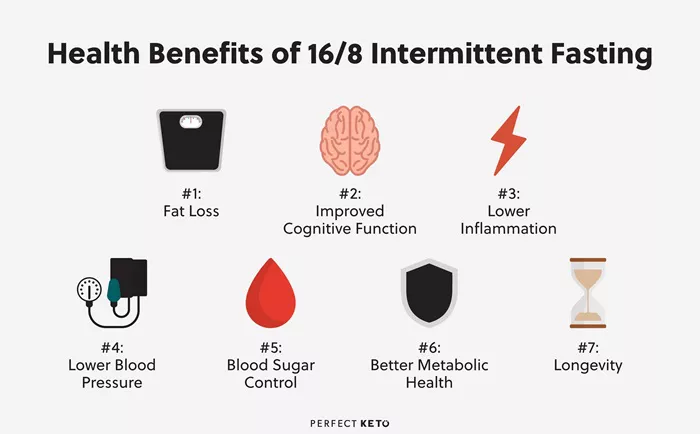
“We have learned lessons from everything that has happened,” Dr. Austin said. “HPV screening is now in operation, and laboratory services have been centralized. Other improvements have been made across the system.”
The review also found that, out of four screeners involved, one has been suspended, and another has had conditions placed on their practice following hearings by the Health and Care Professions Council.
Failures in Management and Oversight
The issues at Southern Health Trust were further compounded by failures in management and accountability. A report by the Royal College of Pathologists (RCPATH) criticized the trust for its “persistent underperformance” and the inadequate handling of staff performance issues.
The report revealed that policies for dealing with underperforming staff were insufficient, and the screening laboratory was not sustainable. The lack of action over many years resulted in missed diagnoses and delays in treatment for affected women.
Since the review, the Northern Ireland health system has made improvements, transitioning from cytology-based screening to primary HPV screening, which is more effective at detecting abnormalities and is expected to identify up to 90% of cases.
Calls for Public Inquiry
The revelations have led to growing calls for a public inquiry into the handling of cervical screening at Southern Health Trust. While some officials, such as Joanne McClean, Director of Public Health at the Public Health Agency, expressed sympathy for the affected women, the decision on whether to launch a public inquiry remains with the health minister.
“It has been an incredibly difficult time for those affected,” McClean said. “The hurt, distress, and grief that people have suffered is deeply regrettable.”
Moving Forward
The findings of the review will undergo an independent expert assessment by Allan Wilson, a senior biomedical scientist with over 45 years of experience in the cervical screening program. This expert review will inform the health minister’s decision on whether a public inquiry is warranted.
Meanwhile, the introduction of HPV screening is expected to improve the accuracy and sensitivity of cervical cancer detection across Northern Ireland. Health authorities are hopeful that these changes will prevent future failings in the screening process.
Symptoms of Cervical Cancer
Women are advised to be aware of the following symptoms, which may indicate cervical cancer:
- Unusual vaginal bleeding, including bleeding between periods, after sex, or after menopause.
- Changes in vaginal discharge.
- Pain during sex or in the lower abdomen, lower back, or pelvic area.
Cervical screening remains a crucial part of early cancer detection, and experts continue to urge women to attend regular screenings to ensure early diagnosis and treatment.
Related Topics
Disputes Between Medicare Advantage Plans and Providers Leave Older Adults Struggling
Health Officials Investigate Pinellas County School After Teacher’s Death from Rare Disease
New Mental Health and Addictions Emergency Care Space to Be Built at Thunder Bay Hospital