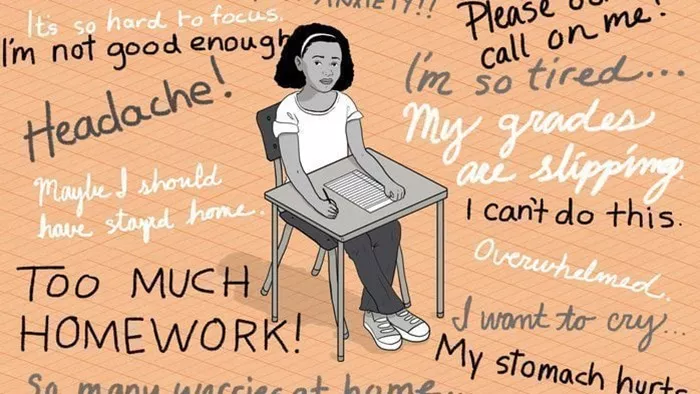
MANKATO, Minn. — The mental health of children has been deteriorating over the past decade, exacerbated by the pandemic, according to a new report from the Center for Rural Policy and Development (CRPD). This report underscores the increasing difficulty for families in rural areas to access mental health services due to logistical challenges and a shortage of professionals.
Marnie Werner, CRPD’s Vice President of Research & Operations, spearheaded the report after recognizing the unique obstacles faced by rural families. “Rural health, overall, is adequate, but barriers in these areas create significant challenges for families seeking help,” Werner explained. The CRPD, established in the 1990s to provide non-partisan data on policy issues across greater Minnesota, has identified a troubling trend in mental health among children, particularly girls.
Data reveals that 35% of survey respondents reported mental health issues in 2019, a figure that surged to 45% by 2022. Werner notes that “mental health” differs from “mental illness” as it encompasses emotional, psychological, and social well-being, impacting how individuals think, feel, and act.
The report highlights several challenges, including long wait times, limited clinic availability, and a shortage of mental health professionals. Additionally, the stigma surrounding mental health continues to hinder many from seeking help. Montevideo Public Schools Superintendent Wade McKittrick noted that children often feel isolated in their struggles, which can prevent them from reaching out for assistance.
In response to these challenges, Werner’s report offers three key recommendations for immediate action:
1. Utilize Existing Educational Resources: Werner emphasizes that knowledge can help alleviate fears. The report points to resources from the National Alliance on Mental Illness, the Minnesota Department of Health, and the Minnesota Association for Children’s Mental Health.
2. Leverage School-Based Services: Many schools in the state now offer mental health services, supported by a state grant that funds therapists in nearly every county. This approach helps reduce the stigma associated with seeking help by providing services within the school environment.
3. Integrate Mental Health into Primary Care: The Minnesota Department of Health’s Office of Rural Health and Primary Care reports that a significant percentage of both urban (83%) and rural (89%) physicians already incorporate some mental health services into their practices. This integration allows for immediate connections to mental health support without requiring visits to specialized clinics.
Werner stressed the importance of these solutions, noting that while long-term improvements will take time, these immediate actions can provide significant relief for rural families. “These shortcuts can help break down barriers when time is critical,” Werner said.
[inline_related_posts title=”You Might Be Interested In” title_align=”left” style=”list” number=”6″ align=”none” ids=”12337,12333,12288″ by=”categories” orderby=”rand” order=”DESC” hide_thumb=”no” thumb_right=”no” views=”no” date=”yes” grid_columns=”2″ post_type=”” tax=””]