Scars are a natural part of the body’s healing process after tissue injury. Whether from surgery, injury, burns, or acne, scars represent the body’s remarkable ability to repair itself. However, the formation and appearance of scars can vary significantly based on several factors, including the nature and extent of the injury, genetic predisposition, and the location on the body. In this article, we delve into the intricate biological processes behind scar formation and explore the various methods used to manage and treat scars.
The Biology of Scar Formation
Stages of Wound Healing
The formation of a scar is the final stage in the complex process of wound healing, which can be divided into four distinct phases: hemostasis, inflammation, proliferation, and remodeling.
Hemostasis: This is the initial response to injury, where the body works to stop bleeding through blood clot formation. Platelets play a critical role in forming a clot, which acts as a temporary barrier to protect the wound.
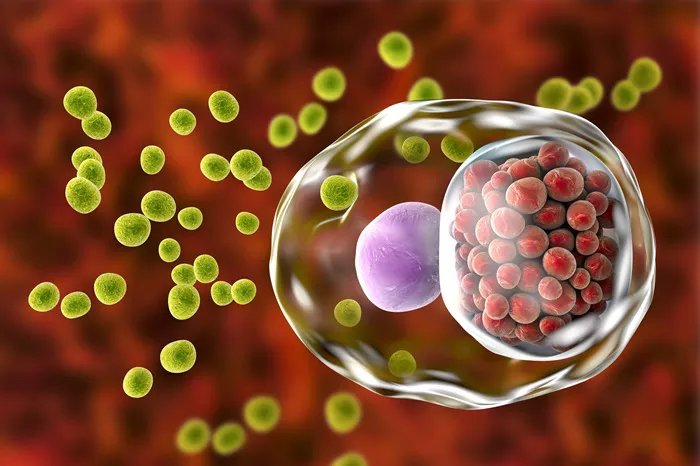
Inflammation: Following hemostasis, the inflammatory phase begins. During this phase, the body sends white blood cells (leukocytes) to the wound site to fight off any potential infections. This stage is characterized by redness, heat, swelling, and pain.
Proliferation: In this phase, new tissue and blood vessels are formed. Fibroblasts are key players, producing collagen and extracellular matrix to provide structural support to the new tissue. This phase includes wound contraction, where the edges of the wound are pulled together to close the gap.
Remodeling: The final phase involves the maturation and reorganization of collagen fibers in the wound. This process can take several months to years, during which the new tissue gains strength and flexibility. The scar tissue that forms is usually less elastic and more fibrous than the original tissue.
Types of Scars
Not all scars are the same. They can vary in appearance and severity based on how the wound heals. Common types of scars include:
Hypertrophic Scars: These are raised scars that remain within the boundaries of the original wound. They often appear red and thick but may improve over time.
Keloid Scars: Unlike hypertrophic scars, keloids extend beyond the original wound boundaries. They are typically raised, thick, and can be itchy or painful. Keloids result from an overproduction of collagen during healing.
Atrophic Scars: These scars are characterized by a depression or indentation in the skin. They often occur after acne or chickenpox, resulting from the loss of underlying structures such as fat or muscle.
Contracture Scars: These occur when a large area of skin is damaged, often from burns. As the wound heals, the skin tightens (contracts), which can restrict movement, especially if located near a joint.
Factors Influencing Scar Formation
Genetic Factors
Genetics play a significant role in how scars form and heal. Some individuals are more prone to developing hypertrophic or keloid scars due to their genetic makeup. Research has identified specific genes and genetic pathways involved in the regulation of collagen production and wound healing.
Skin Type and Color
Skin type and color can influence scar appearance. For instance, individuals with darker skin tones are more likely to develop keloid scars. The increased melanin production in darker skin can also lead to hyperpigmentation around the scar area.
Location of the Wound
The location of the wound on the body can affect scar formation. Areas with higher tension, such as the chest, back, and shoulders, are more prone to developing hypertrophic scars due to the constant movement and stretching of the skin.
Age
Age is another factor that impacts scar formation. Younger individuals tend to heal more quickly and with less scarring compared to older adults. However, young skin is more prone to overactive healing, potentially leading to hypertrophic or keloid scars.
Scar Treatment and Management
While scars are a natural part of the healing process, various treatments and interventions can help minimize their appearance and improve skin function. Treatments can range from topical applications and non-invasive procedures to surgical interventions.
Topical Treatments
Silicone Gel and Sheets: Silicone-based products are widely used to treat hypertrophic and keloid scars. They work by hydrating the scar tissue and reducing collagen production. Silicone sheets or gels are applied directly to the scar and can significantly improve the appearance over time.
Topical Steroids: Steroid creams or injections can reduce inflammation and slow down collagen production, making them effective for treating hypertrophic and keloid scars. However, long-term use should be monitored to avoid potential side effects.
Scar Creams and Ointments: Over-the-counter and prescription creams containing ingredients like onion extract, vitamin E, and aloe vera can help improve the appearance of scars. These products work by moisturizing the skin and promoting collagen remodeling.
Non-Invasive Procedures
Laser Therapy: Laser treatments can help reduce the redness, thickness, and texture of scars. Different types of lasers, such as ablative and non-ablative lasers, target various aspects of the scar tissue. Fractional lasers are particularly effective for treating atrophic scars.
Microneedling: This procedure involves using fine needles to create micro-injuries in the scar tissue. These micro-injuries stimulate the body’s natural healing response and promote collagen production, leading to smoother and more even skin.
Cryotherapy: Cryotherapy involves freezing the scar tissue with liquid nitrogen. It is often used for treating keloid scars by reducing their size and improving their texture.
Dermabrasion: This technique uses a rotating instrument to remove the outer layers of skin, which can help smooth out raised scars and improve their appearance. It is commonly used for acne scars.
Surgical Interventions
Scar Revision Surgery: For more severe scars, surgical removal or modification may be necessary. Scar revision surgery involves cutting out the scar tissue and re-closing the wound with precise suturing techniques to minimize future scarring.
Skin Grafting: In cases of extensive tissue loss, such as severe burns, skin grafting may be required. This involves transplanting healthy skin from another part of the body to cover the damaged area.
Z-Plasty and W-Plasty: These are surgical techniques used to change the direction of a scar, making it less noticeable. Z-Plasty involves creating small triangular flaps of skin that are rearranged, while W-Plasty involves a series of small, zigzag incisions to break up the straight line of the scar.
Emerging Treatments
Stem Cell Therapy: Research into stem cell therapy for scar treatment is ongoing. Stem cells have the potential to regenerate damaged tissues and improve the appearance of scars by promoting healthier skin growth.
Platelet-Rich Plasma (PRP) Therapy: PRP therapy involves injecting concentrated platelets from the patient’s blood into the scar tissue. The growth factors in PRP can enhance healing and improve scar texture.
Botox Injections: Botox injections can relax the muscles around the scar, reducing tension and improving the scar’s appearance. This treatment is particularly useful for facial scars.
Preventing Scar Formation
While it may not always be possible to prevent scars completely, certain measures can help minimize their formation and improve healing outcomes.
Proper Wound Care
Clean and Protect the Wound: Keeping the wound clean and covered with a sterile dressing can prevent infection and promote optimal healing conditions. Regularly changing the dressing and using antibiotic ointments can further reduce the risk of complications.
Avoid Picking or Scratching: Picking at scabs or scratching the wound can delay healing and increase the likelihood of scar formation. It’s important to let the wound heal naturally.
Moisturization and Sun Protection
Hydrate the Skin: Applying moisturizers to the healing wound can keep the skin hydrated and supple, reducing the risk of tight, dry scars. Products containing hyaluronic acid or petroleum jelly are effective choices.
Protect from Sun Exposure: UV rays can darken scars and make them more noticeable. Using sunscreen with a high SPF or covering the scar with clothing can protect it from sun damage.
Massage and Physical Therapy
Scar Massage: Gently massaging the scar tissue can help break down collagen bundles and improve scar flexibility. Using circular motions with a scar cream or oil can enhance the benefits of massage.
Physical Therapy: For scars that restrict movement, especially contracture scars, physical therapy can be beneficial. Stretching and strengthening exercises can improve mobility and reduce scar tightness.
Psychological Impact of Scars
Scars can have a significant psychological impact, affecting self-esteem and body image. Understanding and addressing these emotional aspects is crucial for comprehensive scar management.
Emotional Support
Counseling and Support Groups: Speaking with a mental health professional or joining support groups can provide emotional support and coping strategies for individuals struggling with the appearance of their scars.
Body Positivity: Promoting body positivity and self-acceptance can help individuals embrace their scars as part of their unique story and identity.
Cosmetic Camouflage
Makeup and Concealers: Specialized makeup products designed to cover scars can boost confidence by providing a temporary solution to conceal visible scars.
Tattooing: Medical tattooing or micropigmentation can be used to camouflage scars, particularly for skin conditions like vitiligo or to restore the appearance of eyebrows after surgery.
Conclusion
Scar formation is a complex process influenced by various factors, including genetics, wound care, and the type and location of the injury. While scars are a natural part of healing, numerous treatments and strategies can help minimize their appearance and improve skin function. From topical treatments and non-invasive procedures to surgical interventions and emerging therapies, the options for scar management are diverse and continually evolving.
Understanding the science behind scar repair and the available treatment options empowers individuals to make informed decisions about their care. Whether aiming to reduce the appearance of a scar or seeking to improve mobility and function, a holistic approach that includes proper wound care, prevention strategies, and emotional support can lead to better outcomes and improved quality of life.
[inline_related_posts title=”You Might Be Interested In” title_align=”left” style=”list” number=”6″ align=”none” ids=”8931,8844,8760″ by=”categories” orderby=”rand” order=”DESC” hide_thumb=”no” thumb_right=”no” views=”no” date=”yes” grid_columns=”2″ post_type=”” tax=””]